How Do I Explain My Brain Injury to my Family and Friends?
A concussion and vestibular disorder are “invisible”, as there is no outward injury that is visible to those around you. Unlike a broken leg that involves a cast and crutches, you don’t wear a bandage around your head to indicate that you've had a brain injury. Yet, you may feel horrible and have a hard time explaining why you feel that way.
How do you explain your brain injury to your family and friends?
What is a concussion?
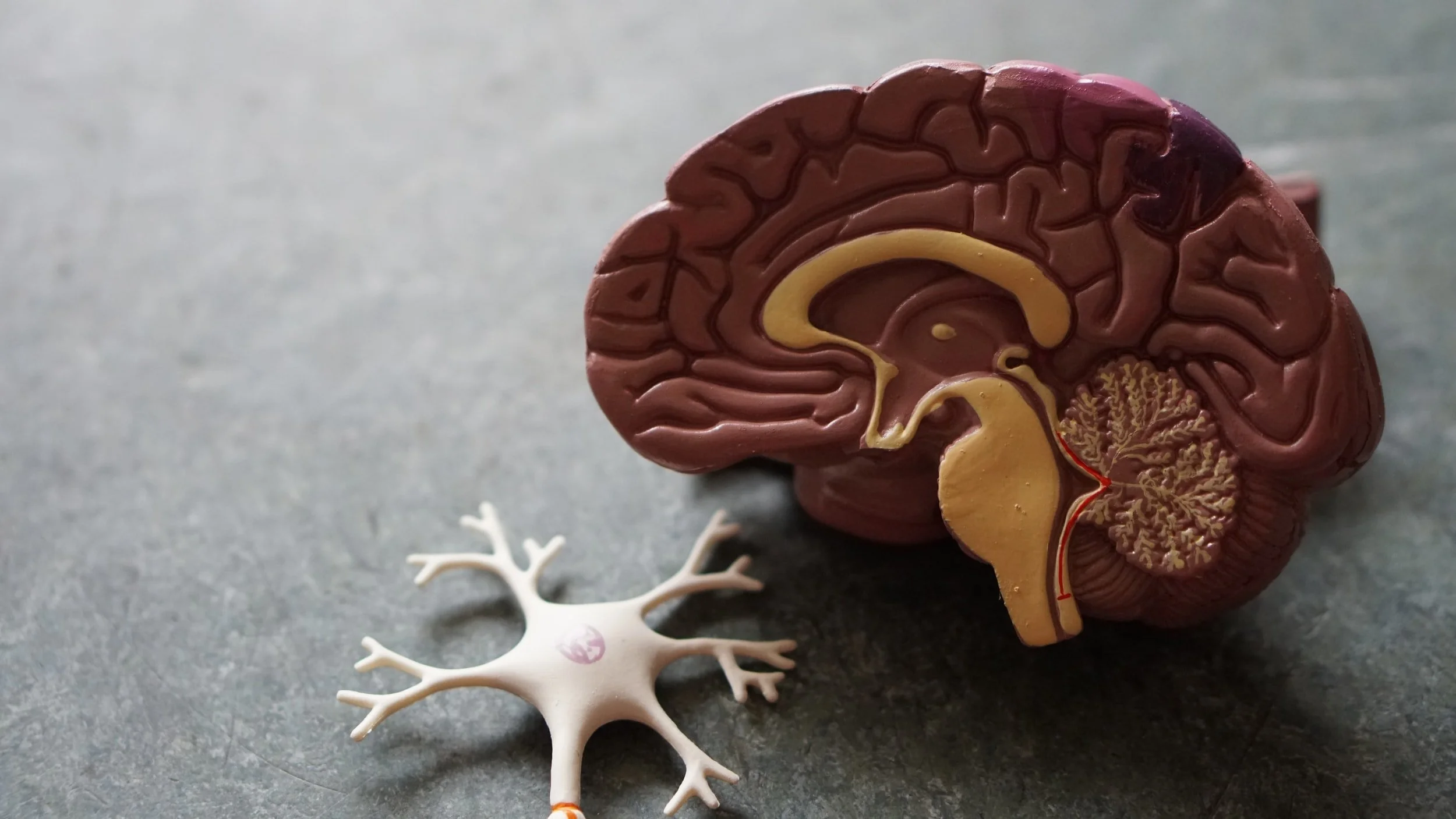
A concussion may involve a direct or indirect hit to the head that results in an acceleration and deceleration force causing shearing and stretching of the neurons in the brain. This causes a functional injury to the pathways resulting in an interruption of the signals going to and from the different areas of the brain. Imaging may not show a lesion in the brain, but it doesn’t mean that the individual is not experiencing symptoms.
What is a vestibular disorder?
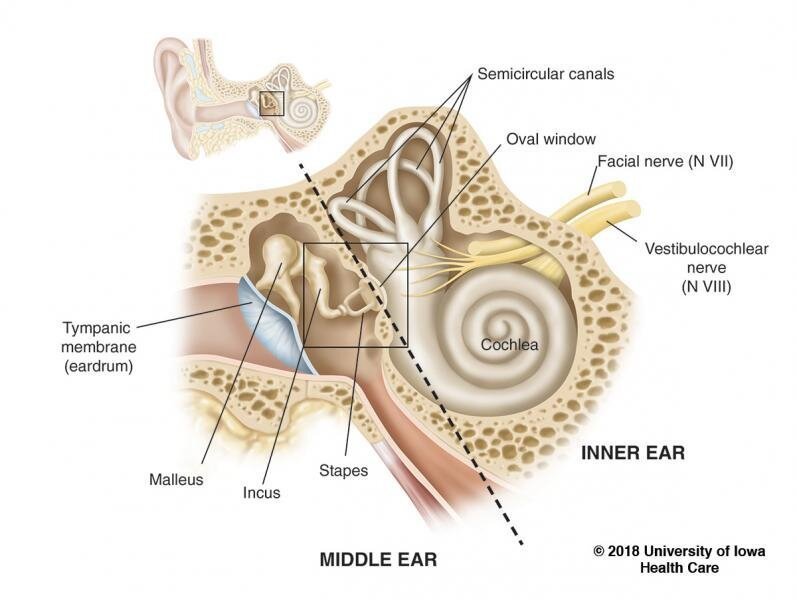
The vestibular system is more commonly known as the ‘inner ear’ and is situated deep within the skull on both sides. The vestibular system involves the peripheral sensory organ, including the cochlea (which is involved with hearing), the nerve going to the brain, and the regions in the brain associated with the vestibular system. The main functions of the vestibular system include gaze stabilization, postural stability, and balance. When one of the structures associated with the vestibular system is affected (e.g. aging, infection, injury, etc.), symptoms can occur.
What symptoms can occur after a concussion or with a vestibular disorder?
A concussion causes an injury to the pathways within the brain resulting in a wide range of symptoms.
Physical symptoms can include:
Nausea and/or vomiting
Sensitivity to noise or light
Balance problems
Difficulty with sleep and feeling more fatigued
Cognitive symptoms can include:
Difficulty thinking clearly
Feeling slowed down
Difficulty focusing and concentrating
Difficulty remembering new information
Difficulty doing more than one task at a time
Emotional symptoms can include:
Irritability
Sadness
More emotional or difficulty managing emotions
Feeling more stressed or anxious
Both sides of the vestibular system need to relay congruent information to the brain in order for you to feel stable. When there is an injury to the vestibular system, mismatched signals from the vestibular systems can cause the following symptoms:
Vertigo: related to the sensation that the person or the environment around them is moving, when they are not actually moving
Dizziness: a vague symptom to describe a wide range of sensations, including feeling faint, lightheaded, woozy, and “off”
Imbalance: difficulties with maintaining equilibrium, potentially resulting in many trips and/or falls
Many of these symptoms are felt by the individual, but cannot be seen by others around them. These symptoms can occur at varying degrees between individuals and can fluctuate over the duration of the individual’s recovery. Different kinds of triggers can bring on specific symptoms and may change day to day.
Why do these symptoms affect daily activities?
These symptoms can make it difficult to perform daily activities, as they can affect the individual’s physical and cognitive tolerance.
It is not that the individual is physically incapable of performing the task, but that the task brings on symptoms that make it difficult to complete the task as easily as before. The individual may require frequent breaks or modifications to the task to make it easier to complete.
Let’s use washing dishes as an example. Washing dishes involves cutlery and dishes banging into each other, which can cause noise sensitivity. It also involves looking down, which can aggravate neck pain and headaches. Moreover, it can cause dizziness as it involves the repetitive turning of your head between the sink and the counter. On top of all of that, you have to stand for long periods of time if you have many dishes to clean! The individual may want to wear earplugs to reduce their noise sensitivity, take frequent sitting breaks, wash only a few dishes at a time, or use a standing stool.
Pacing and planning is a crucial principle that individuals with a brain injury use to schedule their days. It allows them to prioritize their tasks and determine what they are able to accomplish each day, in order to manage their symptoms and prevent burnout. It is not that they are “lazy” and don’t want to do everything that they need to do each day, but rather, that they have less energy available to them to use on a day-to-day basis.
Think of one’s energy levels as a fuel gauge. An individual without a brain injury is a lightweight hybrid vehicle. Their fuel tank can take them further, they don’t have to fill up as often, and they have a backup source of energy. An individual with a brain injury is a heavyweight Hummer. They require more fuel consumption to accelerate to the same speed, therefore requiring more fuel refills. These types of vehicles are inefficient and not meant for everyday use.
Individuals with a concussion or vestibular disorder use different types of strategies to manage their symptoms in order to be able to perform their daily activities. These strategies can vary from person to person, and from day to day. Again, they are not making excuses to not perform their daily activities, but are prioritizing what they are capable of doing each day so that they can have enough fuel in their tank for the next day!
Why do these symptoms last for a long time?
Following a concussion, there is a number of reasons why symptoms can persist beyond the typical recovery period of 1 to 2 weeks, including the severity of the initial injury and symptoms, reduced participation in active rehabilitation earlier on in the recovery process, having pre-existing mental health problems, having a history of migraines and/or headaches, among many other factors.
When symptoms persist, it is likely due to a secondary issue related to the concussion in one or more of the following areas:
Autonomic/Physiological: related to poor blood flow regulation to the brain
Metabolic/Inflammatory: a brain injury can cause an inflammatory process that can perpetuate brain and gut inflammation
Visual/Vestibular: related to impairments with vision, spatial orientation, and spatial awareness
Cervical Spine: concussions are often accompanied by a whiplash injury
Psychological: it could be a pre-existing issue that is exacerbated or can be a new issue resulting from the concussion injury
As for vestibular disorders, depending on the type of condition, symptoms can subside after one treatment session or can fluctuate over time. For example, with Benign Paroxysmal Positional Vertigo, vertigo can subside following a repositioning maneuver, with residual dizziness and imbalance being resolved over time with Vestibular Rehabilitation. Whereas, with Ménière’s disease, symptoms can come and go depending on changes in the body’s fluid volume and electrolyte composition. Moreover, a process called decompensation can occur, where symptoms can return months or even years after symptoms go away. This can be due to a myriad of reasons, including increased stress, poor sleep, or illness. Furthermore, when it comes to Vestibular Rehabilitation, it’s important that the exercises be continuously progressed until the challenges met during daily activities are addressed. If Vestibular Rehabilitation is stopped too soon or if the exercises plateau in difficulty level, then symptoms can persist during certain types of activities and movements that were not addressed in the rehabilitation process.
Because of the persistent nature of these symptoms, individuals may focus on them and devote a significant amount of their time figuring out what they mean and what to do about them. Unfortunately, the medical system can be fragmented, which makes it difficult for individuals to find clear answers to their medical issues. It is important to be mindful that although the individual seems to be “obsessed” with their symptoms, it is not because they are “negative” - it is because they are advocating for themselves and looking for answers.
Do treatments help these symptoms?
An active rehabilitation approach is the most beneficial for recovery from a concussion or vestibular disorder. Furthermore, as many areas may be affected (noted above), a multi-disciplinary approach to treatment is of utmost importance. Although it is important to work with clinicians who specialize in the condition (i.e. concussions or vestibular disorders), it is equally as important to work with clinicians from different disciplines who can address the different areas appropriately, e.g. Physical Therapist, Naturopath, Vestibular Therapist, Neuro-Optometrist, Manual Therapist, Psychologist, etc. This may be why the individual attends multiple appointments throughout the week. Going to these appointments becomes a full-time job, as they are primarily focused on their recovery. Also, because they may not be able to tolerate going to more than one appointment a day (perhaps because of fatigue), they may have an appointment every single day of the week.
The principle of neuroplasticity is the foundation of active rehabilitation. Neuroplasticity is the ability of the brain to reorganize itself by forming new neural connections and pathways throughout life. It allows us to compensate for injuries and diseases that we may encounter throughout our lives so that we can respond differently to new situations and changes in our environment. Although rest is important for recovery, ultimately active treatment approaches are what will promote improved communication between affected brain regions and consequently, improve the symptoms associated with those areas.
You may have noticed that the individual may change clinicians throughout their recovery. It may be that their needs change as their symptoms and issues evolve. Although the treatment approach that is provided by the clinician is important to consider, it is also important for the individual to have a rapport with their treatment providers. Recovery is a vulnerable period of time and working with a competent clinician whom the individual is compatible with can make a huge difference. They need to feel safe in order to heal. So, they may be searching for the right provider to meet their recovery and safety needs.
As a friend or family member of someone suffering from a concussion or vestibular disorder, how can you best support them on their journey to recovery?
Acknowledge that they are suffering from an “invisible” condition, including all of their emotions and pain
Listen to their story and experiences and let them share as much or as little as they want
Try not to make assumptions about how they are feeling and provide a diagnosis of your own
Learn what their triggers are to help them manage them (i.e. light and noise sensitivity, excessive visual motion, busy patterns and backgrounds)
Express willingness to accompany them to their medical appointments
Offer to help them create a list of questions to bring to appointments
Support them with living an overall healthy lifestyle to promote recovery
Offer to help with everyday tasks…
…however, don’t do everything for them
Don’t take their behaviours personally
Educate others about the “invisible” nature of concussion and vestibular conditions
Encourage them to perform a little more every day without being forceful
Highlight the progress and positive aspects of the recovery…
…but be patient and understanding if they are struggling and are experiencing setbacks