What is an Inner Ear Infection (Vestibular Neuritis and Labyrinthitis)?
Vestibular Neuritis and Labyrinthitis involve inflammation of the nerves that connect the inner ear to the brain. Due to the inflammation, the transmission of sensory information from the inner ear to the brain becomes disrupted, resulting in vertigo, dizziness, imbalance, vision problem, and potentially hearing.
The cause of the inflammation may be due to infections of the inner ear and can be of viral or bacterial origin. Inner ear infections are not the same as middle ear infections, which are commonly seen in children. Middle ear infections are usually a type of bacterial infection that affects the area around the eardrum. However, it is possible that chronic, untreated middle ear infections can result in inflammation spreading to the inner ear, resulting in the same symptoms as an inner ear infection.
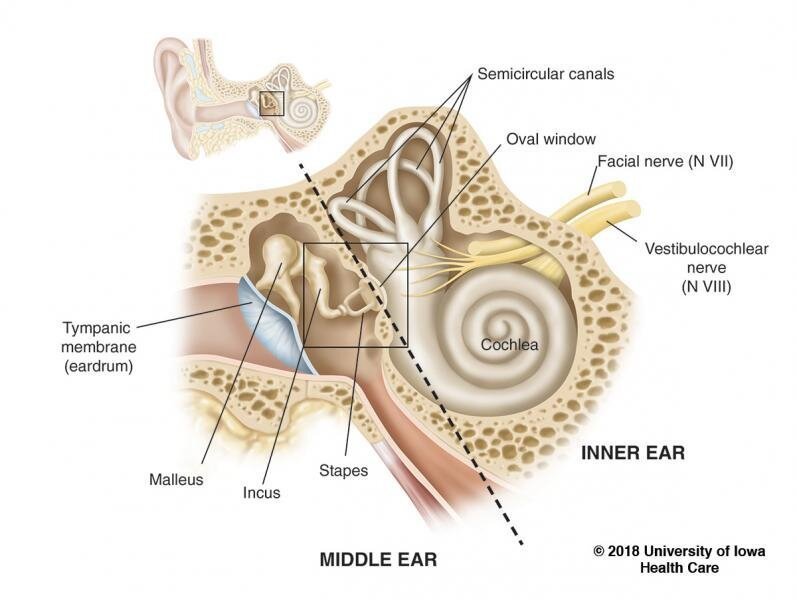
What is the Anatomy of the Inner Ear?
The inner ear consists of a system of fluid-filled tubes and sacs called the labyrinth. The labyrinth serves two functions: hearing and balance.
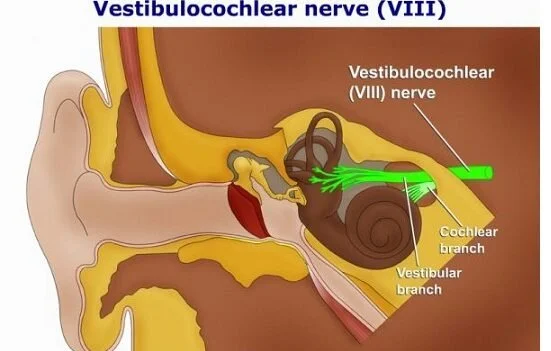
From the labyrinth, signals travel to the brain via the vestibulo-cochlear nerve, which is the 8th cranial nerve. The vestibulo-cochlear nerve has 2 branches:
The vestibular nerve transmits information from the vestibular organs. Fluid and hair cells in the 3 semicircular canals and the sac-shaped utricle and saccule provide the brain with information about head movement.
The cochlear nerve transmits information from the hearing organs. A snail-shaped fluid-filled tube provides the brain with information about sounds.
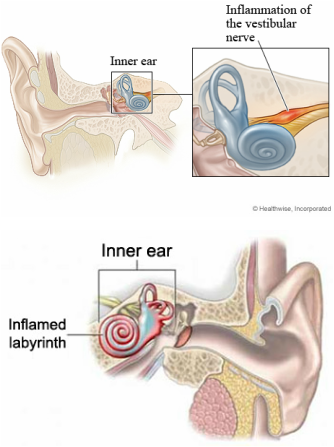
What is the Difference Between Vestibular Neuritis and Labyrinthitis?
Neuritis (inflammation of the nerve):
Neuritis is inflammation of the branch of the nerve associated with balance, the vestibular nerve. The brain integrates the afferent signals sent from the vestibular nerves from the right and the left ear, such that when one side is infected, mismatched signals are sent to the brain. This results in the sensation of dizziness or vertigo, but there will not be a change in hearing.
Labyrinthitis (inflammation of the labyrinth):
Labyrinthitis is inflammation of the branch of the nerve associated with hearing, the cochlear nerve. This also results in the sensation of dizziness or vertigo, but there will also be a change in hearing, such as tinnitus (ringing in the ears), noise sensitivity, or hearing loss.
What are Causes of Vestibular Neuritis and Labyrinthitis?
Inner ear infections that cause vestibular neuritis or labyrinthitis are usually of viral origin, rather than bacterial. Although the symptoms of viral and bacterial infections may be similar, the treatments to properly address them are very different, so accurate diagnosis by a physician is crucial.
Viral
An inner ear viral infection may be the result of a systemic viral illness or the infection may be isolated to the labyrinth or the vestibulo-cochlear nerve, and typically, only one ear is affected.
Viruses that have been associated with causing vestibular neuritis or labyrinthitis include herpes viruses (such as the ones that cause cold sores, chicken pox, or shingles), influenza, measles, rubella, mumps, polio, hepatitis, and Epstein-Barr. If an inner ear infection is caused by a virus, it can run its course and then go dormant in the nerve, only to flare up again at any time. Thus, there is currently no way to predict whether or not it will come back.
Bacterial
An inner ear bacterial infection may be the result of bacteria that has infected the middle ear or the bone surrounding the inner ear, producing toxins that invade the inner ear via the oval or round windows. The toxins cause inflammation to the cochlea, the vestibular system, or both. This is called serous labyrinthitis and is most commonly a result of chronic, untreated middle ear infections (chronic otitis media) that is characterized by milder symptoms.
An inner ear bacterial infection may also be the result of suppurative labyrinthitis, which occurs when bacterial organisms invade the labyrinth. The infection originates either in the middle ear or in the cerebrospinal fluid (i.e. bacterial meningitis). Bacteria can enter the inner ear through the cochlear aqueduct or internal auditory canal, or through a fistula (abnormal opening) in the horizontal semicircular canal.
What are the Symptoms of Vestibular Neuritis and Labyrinthitis?
Symptoms can range from mild to severe, including dizziness, vertigo, nausea, vomiting, imbalance, vision problems, and impaired concentration. In some case, the symptoms can be so severe that they affect the ability to stand up or walk. With vestibular labyrinthitis, there is also tinnitus, noise sensitivity, and/or hearing loss.
Acute Phase
In the acute phase, the onset of symptoms is very abrupt, with severe dizziness or vertigo coming on suddenly, such that it is extremely frightening and anxiety-provoking for the individual. Many times, the individual goes to the emergency room or sees their family physician on the same day, due to the severity of the symptoms.
Chronic Phase
In the chronic phase, which is usually several weeks later, the symptoms have gradually reduced to the point that the individual can return to some activities of daily living. At this time, if there are residual symptoms, they would benefit from being addressed with Vestibular Rehabilitation. Unfortunately, there could be chronic dizziness if the virus caused damage to the vestibular nerve. However, with Vestibular Rehabilitation, compensatory strategies can be developed to manage chronic dizziness and imbalance.
Other symptoms that become apparent during the chronic phase include:
Fatigue
Visual motion sensitivity (i.e. moving cars, being in crowds)
Brain fog or haziness
Issues with focus and concentration, including multi-tasking
How Do You Diagnose Vestibular Neuritis and Labyrinthitis?
There are no specific tests that can confirm the diagnosis of vestibular neuritis or labyrinthitis. It is usually a diagnosis of exclusion, meaning that a series of tests are conducted to eliminate other potential causes of the same symptoms, such as stroke, head injury, cardiovascular disease, allergies, side effects of prescription or nonprescription drugs (including alcohol, tobacco, caffeine, and many illegal drugs), neurological disorders, and anxiety.
If symptoms persist, additional testing may be required to help determine whether a different vestibular disorder could be the cause of the persistent symptoms. These tests can include an audiogram (hearing test), electronystagmography (ENG), or videonystagmography (VNG), which may include a caloric test to measure any differences between the function of the two sides of the vestibular system. Vestibular-evoked myogenic potentials (VEMP) may also be performed to detect damage in a particular portion of the vestibular nerve.
How Do You Treat Vestibular Neuritis and Labyrinthitis?
Treatment during the acute phase
Initially, medications are typically prescribed to control the acute symptoms, including nausea and dizziness, and to treat the cause of the infection, such as steroids (e.g., prednisone), antiviral drugs (e.g., Acyclovir), or antibiotics (e.g., amoxicillin).
If the treatment is provided in a timely manner, the infection will not cause permanent damage to the vestibulo-cochlear nerve. In some cases, if there is damage to the nerve, permanent damage to the vestibular system or permanent loss of hearing can occur. Following vestibular neuritis or labyrinthitis, it can make one more susceptible to Benign Paroxysmal Positional Vertigo (BPPV) or endolymphatic hydrops (abnormal fluctuations in the inner ear fluid called endolymph).
Treatment during the chronic phase
In the chronic phase, which is typically several months following the initial onset of symptoms, Vestibular Rehabilitation may be beneficial to address persistent symptoms, including dizziness and imbalance. Vestibular Rehabilitation retrains the brain’s ability to adjust to the change in signals from the inner ear to the brain.
Individualized Vestibular Rehabilitation exercises are prescribed that can be performed independently and safely at home. It is important that the exercises are closely monitored at the beginning, as they can be quite symptom-provoking. It is crucial that the exercises provoke a mild level of symptoms to initiate adaptations in the vestibular system, but are not at a severe intensity, such that the individual is unable to carry on with their daily activities. When Vestibular Rehabilitation commences, it is usually recommended that vestibular-suppressant medications be discontinued, as they can interfere with the ability of the brain to adjust to the exercises.
The Vestibular Rehabilitation exercises may provide immediate relief, but a considerable difference may not be evident for several weeks. Oftentimes, people find they must continue the exercises, even if their symptoms have resolved, in order to maintain optimum inner ear function. Others may find that they can stop doing the exercises altogether, without experiencing any problems. Besides the Vestibular Rehabilitation exercises, it is crucial that a general exercise program (i.e. walking, strengthening exercises) is established in an effort to maintain physical activity, as being sedentary can prolong the recovery process or increase the risk of re-occurrence of symptoms.
If permanent damage to hearing has occurred, hearing aids may be useful. Treatment for tinnitus may also be considered, if prominent.
Why is it so difficult to describe my symptoms?
With vestibular neuritis or labyrinthitis, it is difficult to describe symptoms due to the generalized nature of the symptoms and variability in the intensity of the symptoms as the condition progresses. Also, you may not associate your symptoms with a precipitating cause, such as a viral or bacterial infection, as the symptoms may be delayed. Furthermore, because you may look healthy and well, it is difficult to explain to someone else how you may be feeling, as you do not “have something to show for it”, such as a broken arm. It is distressing because until you learn why you are feeling this way, you feel like you should be able to continue to perform your daily activities, despite it being difficult for you to carry them out. As a result, you may become depressed or anxious, as you realize that you are unable to perform your daily activities at your previous capacity.
Seeing a medical professional who specializes in vestibular disorders and hearing from others who may be going through the same things are important steps towards learning more about the condition and your recovery!